WHAT ARE SYMPTOMS OF ROOT CANAL AND WHAT IS ROOT CANAL TREATMENT?
Tooth pain is frequently a marker of major dental problems; however, a toothache does not always indicate the necessity for a root canal. Self-diagnosis is a poor method that can lead to the need for tooth extraction if excessive time passes before an expert diagnosis. In this scenario, self-assurance might lead to a significant mistake, resulting in extreme pain and losing one tooth. However, one less tooth is hardly the most frightening effect of a delayed toothache, and recent history has cases where a minor toothache became lethal. This article talks about what is root canal, its cause, symptoms, and treatment.
What is a Root Canal?
Root canals contain blood vessels that give teeth nutrition and nerves that detect influencing variables such as cold, heat, and pressure. The term “root canal” is defined in two distinct ways; one refers to the inner tooth located between the tooth roots and the pulp. The second relates to tooth care focused on removing infectious material and alleviating toothache. (its root canal treatment the 2nd one that is written does not mean root canal)
What causes root canal infection?
A root canal infection can occur for various causes, but the underlying cause is bacterial penetration into the pulp. The manner bacteria invade the tooth pulp determines the cause of root canal infections. The following are some of the causes of root canal infection:
- Dental decay (caries) causes germs to infiltrate and infect the pulp.
- A fractured or damaged tooth that allows bacteria to enter pulpal tissue.
- Concussion-induced sterile necrosis (signs include tooth discoloration or highly calcified canals, identified by x-ray).
- A defect in tooth anatomy that allows germs to infect the pulp tissue.
The most common cause of a root canal infection is caries, which destroys the tooth and allows germs to enter and infect the pulp. Hence, it is essential to prevent pulp infections; it is critical to detect and eradicate caries as soon as possible.
Symptoms for root canal
Symptoms identified by patients
Only qualified dentists can use professional methods to determine the need for a root canal. However, the following root canal symptoms might prepare patients for what to expect from future dental operations.
- Pain
- Sensitivity
- Swelling,
- Gum Tenderness
- Pus Drainage
There is certainly an issue if the patient suffers from one or more of these symptoms. Each attribute must be thoroughly examined to establish whether a root canal is required.
Symptoms identified by Dentists
After listening to the patient’s symptoms and concerns, a dentist will utilize expert procedures to determine whether endodontic therapy is warranted. Dentists use the following approaches to suggest the need for a canal root:
- X-Rays: The patient has to discover what causes a root canal; if a bad tooth causes no pain or swelling, they may not even realize that they require immediate dental care. Dentists utilize x-rays to detect a radiolucency, a dark patch on the tip of the affected tooth that signals that bone changes have already occurred due to the infection inside the tooth. As a result, regular x-ray screenings can detect potential dental problems early, allowing the patient to apply effective treatment options.
- Gum Boils: Dentists look for the existence of gum boils, which are medically known as fistulous tracts. These pus drains allow pus to drain rather than invade the soft tissues surrounding the tooth. As a result, pus seeks a route out: it can either infiltrate the soft tissues and create swelling or form a drain that leads outside. Pus may induce edema if that drain becomes clogged. Such tracts are frequently painful to the touch, although they may not always signal the necessity for a root canal. Gum disease can also cause a lesion in some situations (periodontal issue).
- Discoloration: Tooth discoloration indicates that there have been alterations within the nerve space. This symptom often signals that root canal therapy is required. The discoloration is frequently caused by tooth trauma. Furthermore, discoloration may occur without the presence of a toothache or swelling. However, a discolored tooth does not always indicate that endodontic therapy is required. This symptom is frequently combined with others to decide the best course of action
- Nerve Exposure: Since it is difficult to identify how close a nerve is to the tooth surface, nerve exposure can occur if a dentist comes into contact with pulp tissue during treatment. In this scenario, a root canal is advised since future tissue deterioration may result from exposure.
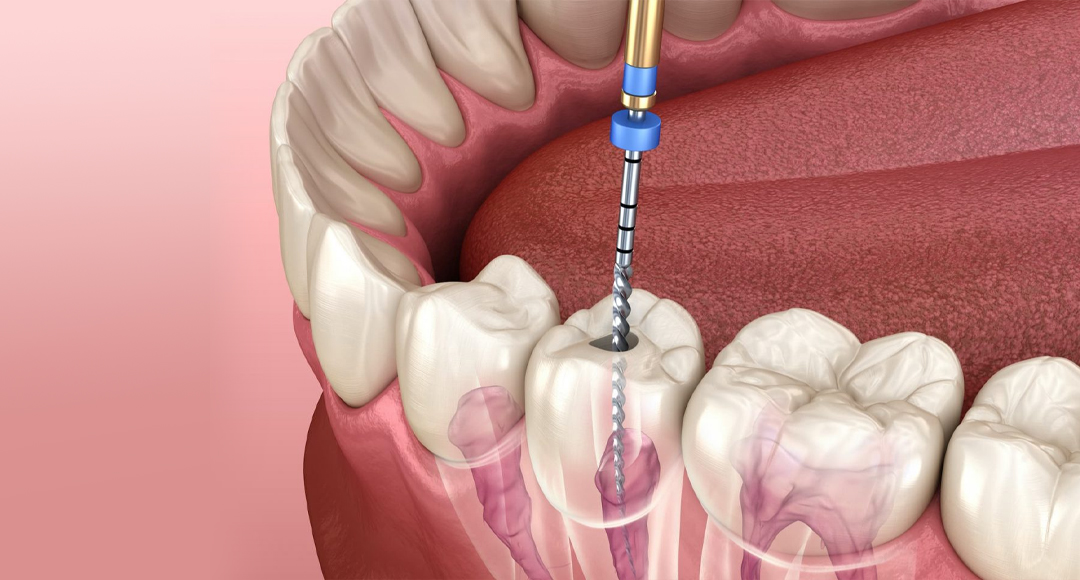
Treatment of Root Canal
Endodontists specialize in root canal therapy; however, Dentists and Endodontists can perform this treatment. Endodontists have greater competence, more practical knowledge, and more experience in this type of therapy because it is their specialty.
The endodontic branch is named after the Greek terms for “within” (“endo”) and “tooth” (“odont”). A root canal is merely one type of endodontic therapy, which refers to the treatment of the soft tissue inside teeth called the pulp, which plays an important part in the development and growth of the tooth. Because of the surrounding tissues, a completely developed tooth can live without the pulp. In this section, we will go over each stage of root canal surgery, including:
- Dental X-Rays: An endodontist can use X-rays to diagnose pulp damage and estimate the form of the root canal. This approach also aids the specialist in determining the location of a tooth infection and bone deterioration.
- Anesthesia: At this point, a professional will use a local anesthetic to minimize any pain that the patient may be experiencing. Even though the inner nerve is usually dead in these cases, a dentist may still use a drug to reduce any pain.
- Placement of the dental dam: A dental dam is a rubber sheet surrounding the problematic tooth to keep it dry. This dam keeps saliva from entering the treated area.
- Making an Incision and Removing the Decayed Pulp: An endodontist makes a hole in the patient’s tooth to reach the diseased pulp. After precisely drilling the spot, the specialist uses root canal cleaning to remove the bacteria-infected pulp. Because an anesthetic is used, this procedure will be painless.
- Opening Medication: A dentist will medication the inside tooth area to eradicate bacteria if the patient’s tooth has an inner infection. The tooth is then filled with a temporary substance until the patient’s next visit. In some circumstances, the hole might be left open until the next stop to allow pus to drain.
- Finishing the Tooth: At this point, the patient’s tooth is sealed off by a dentist. They first replace the temporary material within the patient’s tooth with a permanent replacement before sealing it shut.